Febrile Seizure: Review
Febrile Seizures

What is febrile seizure?
Febrile seizures are seizures that are caused by a sudden spike in body temperature with fevers greater than 38C or 100.4F, with no other underlying seizure-provoking causes or diseases such as the central nervous system (CNS) infections, electrolyte abnormalities, drug withdrawal, trauma, genetic predisposition or known epilepsy.
There shouldn't be any prior history of afebrile seizure as in such case the fever might be the cause of breakthrough seizure. however , there are no consensus regarding inclusion or exclusion of children with neurodevelopment disorder such as Autism spectrum disorder which has the predisposition to seizures.
Age of presentation:
As per American academy of Pediatrics:
6 months to 5 years (however cases unto 7 years of age have been diagnosed as FS)
As per earlier definition ILAE - infant up to age of 1 month can be diagnosed as FS.
As per NIH (National Institute of Health) children between 3 months and 5 years of age are included.
Which age group are particularly affected?
Most common in children between 12 to 18 months of age. 90% of children have their first episode by 3 years of age.
Any gender preponderance:
Although some studies shown male predominance but most studies have shown no effect of gender.
Why age cut off is important?
Now if we include infants unto the age of 1 month - a lot of children with genetic epilepsy syndromes that include Dravet or PCDH19 which can present as febrile seizures below 6 months get included. This will confound the outcome and give a false assertion about febrile seizure related brain injuries.
Similarly if we include children above 6 years - this may again encompass all those children who later on develop epilepsy syndromes associated with fever like GEFS+, Dravet etc..,
Classification:
Simple(SFS) vs Complex (CFS)
Simple febrile seizures are single(within 24 hour), generalized convulsions lasting <15 min.
Complex febrile seizures present with focal features, occur as clusters of episodes during the same 24-h period (multiple seizures) or are prolonged with a duration longer than 15 min or associated with postictal neurologic abnormalities, including Todd paresis or those without the regain of consciousness for more than 1 hour.
CFS often occur in patients with a preexisting neurologic abnormality.
How common are CFS?
Approximately 20–35% of febrile seizures are complex.
What is febrile status epilepticus?
FSE has traditionally been at least 30 minutes of continuous sei- zure activity or 30 minutes of recurrent seizures without full recovery of consciousness in between the seizures. However, as per 2015 ILAE redefined time periods for status epilepticus, including FSE, are as: (1) 5 minutes for generalized tonic–clonic seizures; (2) 10 minutes for focal seizures; and (3) 10 to 15 minutes for absence seizures.
FSE accounts for 25–52% of all status epilepticus in children, although it is a small fraction of febrile seizure occurrences.
FSE have a greater risk of future adverse events up to 41% having febrile seizure recurrence
Children with underlying neurological abnormalities are at a greater risk of having FSE
FS tend to occur more in winter months with Japan(9% of all children) and Guam (14%) having highest incidence rate.
What is Afebrile febrile seizure?
Seizures in an acute infectious illness (particularly gastroenteritis) without documented fever and features consistent with simple FS.
 https://pubmed.ncbi.nlm.nih.gov/15351013/
https://pubmed.ncbi.nlm.nih.gov/15351013/
Which febrile illness has protective effect on febrile seizure?
Gastroenteritis
 https://pubmed.ncbi.nlm.nih.gov/15351013/
https://pubmed.ncbi.nlm.nih.gov/15351013/
What is FS+?
Febrile seizures that continue past the usual age where they are expected to resolve (6 years) and/or accompanied by afebrile generalized or focal seizures.
What is GEFS+?
GEFS+ is an autosomal dominant syndrome with a highly variable phenotype and incomplete penetrance. It can be defined as FS+ with at least 2 family members with FSs, FSs plus, or afebrile generalized or focal seizures.
Risk factor a/w first episode febrile seizure
Why iron deficiency is a/w FS?
Iron is essential for the functioning of certain neurotransmitters, such as monoamine oxidase and aldehyde oxidase. Iron-deficiency anemia may predispose to febrile seizures
Risk factor a/w recurrent febrile seizure

From Nelson
Febrile seizures recur in approximately 30% of those experiencing a first episode, in 50% after two or more episodes, and in 50% of infants younger than 1 yr of age at febrile seizure onset

Having no risk factors carries a recurrence risk of approximately 12%; one risk factor, 25–50%;two risk factors, 50–59%; three or more risk factors, 73–100%.
Seizure threshold is lower in younger children and in those with a family history of febrile seizures.
Risk of febrile seizure recurrence increases when >1 risk factor is present, but the exact effect is uncertain.
Each additional febrile seizure increases the risk of further recurrence, suggesting that experiencing febrile seizures leads to a lower threshold for future seizures
Other epilepsy related risk:
A child who has had a febrile seizure has a greater risk of experiencing afebrile seizures or epilepsy subsequently which infers to the possibility of certain brain abnormality which in the first place predisposed them to FS or it may be the other way around where the FS episodes might prime the brain to recurrent seizures.
Viruses, vaccines and FS
Febrile seizures often occur in roseola and human herpesvirus (HHV) 6 infections; and infections with influenza, RSV, Adeno, rhino, norovirus, enteroviruses
Otitis media is the most common bacterial cause of FS.
In patients with febrile status epilepticus, HHV-6B (more frequently) and HHV-7 infections account for 30% of the cases.
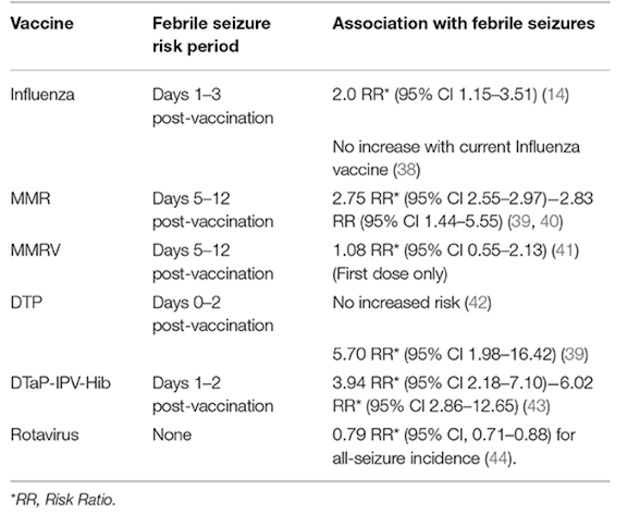
Vaccinations:
Although there is an increase in FS episode with certain vaccination - ultimately they reduce the risk of viral infections which subsequently lower the FS episodes.
Risk of
Although SFS do not have an increased risk of mortality, CFS may have an approximately 2-fold long-term increase in mortality rates, as compared with the general population, over the subsequent 2 yr, probably secondary to a coexisting pathology.
There are no long-term adverse effects of having one or more simple febrile seizures. Compared with age-matched controls, patients with febrile seizures do not have any increase in the incidence of abnormalities of behavior, scholastic performance, neurocognitive function, or attention.
Genetic Susceptibility to Febrile Seizures:
Associations between reduced hippocampal and amygdala size, and families with a greater prevalence of febrile seizures.
These findings suggest that structural malformations of the hippocampi underly the mechanism of febrile seizures (rather than being sequelae of febrile seizures).
Voltage-gated sodium ion channels play an integral role in the propagation of an action potential in neurons. Variations in genes coding for the sodium channel protein have been found, confirmed by the discovery of many sodium channel subtypes. Genes associated with febrile seizures include SCN1A, SCN1B, SCN9A, and CPA6.
In terms of other etiologies, a dysregulation between the proinflammatory IL-1β, IL-6, and IL-8 cytokines and antiinflammatory ILR- 1A cytokines has been associated with febrile status epilepticus.
A decreased ILR-1A/IL-8 ratio (suggestive of an overall proinflammatory state) is predictive of hippocampal abnormalities on MRI done after febrile status epilepticus. The ILR-1A/IL-8 ratio may thus prove to be a potential biomarker for identifying febrile seizure patients who may be at higher risk for developing mesial temporal lobe epilepsy later in life.
Evaluation
Role of Neuroimaging:
No role in case of Simple febrile seizure.
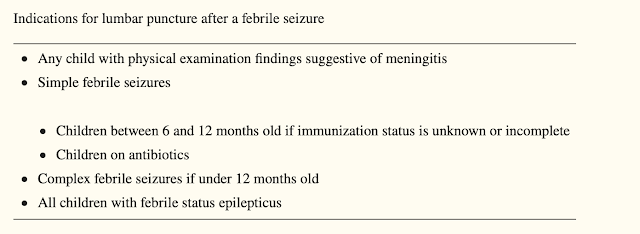
Role of LP:
(Immunization status against HIB and Pneumococcus)
There is no clear evidence to suggest for or against a lumbar puncture among patients with CFS. In general, the literature suggests that although the risk of acute bacterial meningitis with febrile seizures is low, the data are heterogeneous and may be biased toward SFS given the relative incidence of SFS to CFS. Given this, the clinician should consider a lumbar puncture in the context of each individual patient. However, bacterial meningitis should still be an important consideration in the areas without access to adequate immunization and in developing countries
Children with febrile status epilepticus are at higher risk for meningitis compared to those with simple and complex febrile seizures. Studies have documented rates of bacterial meningitis of 12% and 17% with febrile status epilepticus. Two recently published guidelines recommend performing a lumbar puncture on all children with febrile status epilepticus
 https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6052913/
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6052913/
 https://pubmed.ncbi.nlm.nih.gov/30932454
https://pubmed.ncbi.nlm.nih.gov/30932454
Role of Neuroimaging:
The AAP clinical practice guideline advises against routine neuroimaging for children with first SFS but there are no clear recommendations for children with CFS.
Head CT scan is not routinely recommended in the evaluation or management of patients with complex febrile seizures. CT scans may have diagnostic use if there is a strong indication of an acute/subacute bleed or structural lesion based on patient’s exam and history.
Non-urgent, outpatient MRI brain is recommended for patient with focal complex febrile seizures, especially with postictal neurological deficit. Focal complex febrile seizures can be associated underlying structural brain abnormalities and can potentially cause hippocampal atrophy and sclerosis on follow up imaging. There is no evidence to support routine use of neuroimaging in children with CFS without interictal or postictal focality;
However, in febrile status epilepticus there is evidence of hippocampal abnormalities found but this was in patients with febrile seizures greater than 30 minutes and thus not CFS. Urgent brain MRI in the emergency room is not recommended.
 https://pubmed.ncbi.nlm.nih.gov/18356445/
https://pubmed.ncbi.nlm.nih.gov/18356445/
Role of EEG
The AAP recommends against EEG in neurologically healthy children with a SFS. EEG may be useful in complex or atypical features or with other risk factors for the development of epilepsy.
Routine EEG should be considered after a complex febrile seizure. If there is doubt that the event was a seizure, an EEG done on the day of, or shortly after, the seizure may be helpful to clarify.
Otherwise, in regards to timing as a prediction for future febrile and afebrile seizures, the evidence is conflicting thought there is the suggestion that obtaining the EEG within 7 days may increase the likelihood of finding abnormalities although the correlation to the timing of the detection of abnormalities and future prediction ability of epilepsy is unclear.
There was also no clear evidence that particular EEG findings or abnormalities are able to predict the risk of development of epilepsy; rather the persistence of EEG abnormalities had more predictive value. However, future studies are needed to further clarify the issue.
Treatment
Most cases of SFS do not require acute management as the seizures usually get terminated as child reach ER. In case of continuous seizure as in status epileptics treat as Status.
Prevention:
A 2017 Cochrane review found that continuous treatment with phenobarbital and intermittent treatment with diazepam prophylactically was effective at reducing the recurrence of febrile seizures.However, there were adverse effects in up to 30% of cases, leading the authors to advise against the use of these medications.
Similarly, the AAP advises against the use of continuous and intermittent prophylactic antiseizure medication for febrile seizures.
The AAP has concluded that “although antipyretics may improve the comfort of the child, they will not prevent febrile seizures.
 https://pubmed.ncbi.nlm.nih.gov/18519501/
https://pubmed.ncbi.nlm.nih.gov/18519501/
Only one randomised control study in Japan has shown that rectal acetaminophen may reduce the risk of febrile seizure recurrence within the same febrile episode.
In case of CFS
Intermittent use of phenobarbital and antipyretics, clobazam or rectal diazepam has some evidence supporting its use to prevent recurrence of CFS but the data does not effectively separate SFS from CFS and, thus, there may be a bias due to the relative incidence of the respective seizures (class III).
Use of carbamazepine to prevent recurrent CFS is not recommended given other alternatives available such as phenobarbital.
A study comparing valproate, phenobarbital, and placebo seemed to show benefit from valproate with 4% of recurrence. Again the study is devoid of detailed description of initial seizure and recurrent seizure types and thus clinical correlation should be considered.
An individualized risk-benefit approach is recommended for each patient at this time given the levels of evidence for use of prophylactic AED.
Criteria for Hospital admission:
There is no literature with recommendations regarding when to admit a patient after complex febrile seizure.
Factors to consider include multiple seizures within a 24-hour period and the risk of further seizures, prolonged postictal period and severity or focality of seizure necessitating expedited inpatient evaluation.
Social factors, access to medical services and institutional preferences may also affect the disposition of a patient.





Comments
Post a Comment