CHILDHOOD ABSENCE EPILEPSY
- As per the current International League Against Epilepsy (ILAE) classification system, CAE is classified as an epilepsy syndrome with presumed genetic cause.

- Also k/a Petit Mal epilepsy.
- Usually starts at 5-8 years of age.
- Up to 20 percent of children have a history of febrile seizures and nearly half have a first- or second-degree relative with seizures.
- It is a common generalized epilepsy in children.
- It is characterized as short and frequent episodes of profound impairment of consciousness without loss of body tone, lasting about 10 seconds and occur multiple times in a day.
- The three most common seizure features are pause/stare (80 to 95 percent), motor automatism (40 to 60 percent), and eye involvement (55 percent).
- Atypical absences should be suspected if the duration of the events exceeds the classic 10 to 20 seconds.
- Absence seizures do not have postictal period and are characterized by immediate resumption of what the patient was doing before the seizure.
- Hyperventilation for 3-5 min can precipitate the seizures and the accompanying 3-Hz spike-and–slow-wave discharges.
- Absence epilepsy are not provoked by sensory or visual stimuli.
- No body tone changes during absence seizures.
- Early-onset absence seizures (<4 yr of age) or drug resistance should trigger evaluation for a glucose transporter defect,which is often associated with low CSF glucose levels and an abnormal sequencing test of the transporter gene.
- Children with CAE typically have intact cognition and intellect at the time of diagnosis.
- Higher rates of ADHD, anxiety, depression, social isolation, and low self-esteem in patients with absence seizures compared with healthy subjects.
- The classic EEG finding is Ictal EEG s/o 3 Hz spike and wave discharge with abrupt onset and termination.

- Atypical absence seizures have associated myoclonic components and tone changes of the head (head drop) and body and are also usually more difficult to treat. They are precipitated by drowsiness and are usually accompanied by 1- to 2-Hz spike-and–slow-wave discharges.
- Juvenile absence seizures are similar to typical absences but occur at a later age and are accompanied by 4- to 6-Hz spike-and–slow-wave and poly-spike and–slow-wave discharges. These are usually associated with juvenile myoclonic epilepsy.
- Neuroimaging is not required for diagnosis.
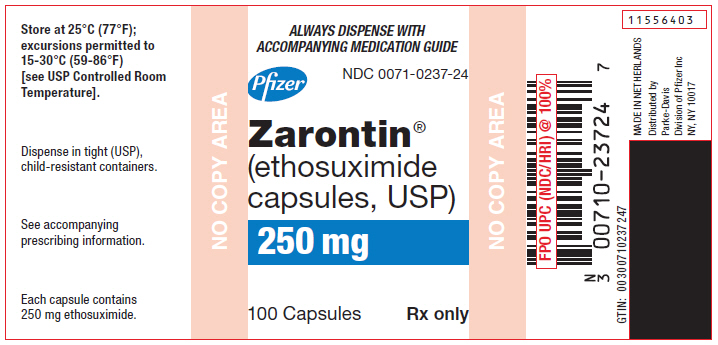
- Ethosuximide is the first line of treatment with starting dose of 5 to 10 mg/kg/day in two divided doses for children younger than six years, and 250 mg twice daily for children age six years and older. The usual maintenance dose is 15 to 40 mg/kg/day in divided doses.
- In patients who have inadequate control of TAS or intolerable side effects on ethosuximide, switch to valproate monotherapy, although lamotrigine may be a better alternative in females of childbearing age based on the increasingly well characterized fetal risks of valproate.
- Additional options for refractory CAE include topiramate, benzodiazepines, acetazolamide, ketogenic dietary therapy, and vagus nerve stimulation.
- Avoid carbamazepine, gabaoentin, vigabatrin.


Comments
Post a Comment