Poliomyelitis
The word poliomyelitis originates from the Greek word “polio” meaning “grey” and “myelon” meaning “marrow.”
Poliomyelitis is an exclusive human disease transmitted from a patient or a symptom-free carrier through the fecal-oral route.
Polio - virus
Mye- spinal cord
itis - inflammation
What type of virus is Polio?
Non-enveloped, positive stranded RNA virus
Belongs to picornaviridae family in the genus Enterovirus species-Enterovirus C
What are the serotypes of Poliovirus?
3 genetically distinct serotypes 1,2, 3
Which type of Polio is maximally associated with Paralytic poliomyelitis?
Type1 poliovirus has the greatest propensity for natural poliomyelitis and type 3 poliovirus has a predilection for producing VAPP.
How does transmission of Polio virus occur?
By feco-oral route and during epidemics via pharyngeal transmission.
What is the incubation period of poliomyelitis?
Usually 8-12 days with a range of 5 to 35 days
What is the pathogenesis of poliomyelitis?
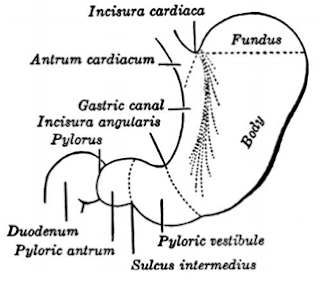
After ingestion, poliovirus is thought to infect epithelial cells in the mucosa of the gastrointestinal tract and then to spread to and replicate in the submucosal lymphoid tissue of the tonsils and Peyer’s patches. The virus next spreads to the regional lymph nodes, a viremic phase ensues, and the virus replicates in organs of the reticuloendothelial system.
In some cases, a second episode of viremia occurs and the virus replicates further in various tissues.
During the primary viremia period patient may manifest flu like symptoms like fever, myalgia, gastroenteritis which in most of the cases subsides or can go on to develop CNS symptoms.
Poliovirus attaches to CD155 receptor on the cells. The virus penetrates the cell, is uncoated, and releases viral RNA. The RNA is translated to produce proteins responsible for replication of the RNA, shutoff of host cell protein synthesis, and synthesis of structural elements that compose the capsid. Mature virus particles are produced in 6-8 hr and are released into the environment by disruption of the cell.

How does Poliovirus gain access to CNS?
It is uncertain whether poliovirus reaches the central nervous system (CNS) during viremia or whether it also spreads via peripheral nerves.
Since viremia precedes the onset of neurologic disease in humans, it has been assumed that the virus enters the CNS via the bloodstream.
Studies demonstrating the poliovirus receptor in the end-plate region of muscle at the neuromuscular junction suggest that, if the virus enters the muscle during viremia, it could travel across the neuromuscular junction up the axon to the anterior horn cells.
How early can we obtain poliovirus for culture from blood?
As early as 3-5 days before the development of neutralising antibosies
How long are poliovirus shed from Gastrointestinal tract of infected individuals?
Poliovirus is shed from the oropharynx for up to 3 weeks after infection and from the gastrointestinal tract for as long as 12 weeks; hypergammaglobulinemic patients can shed poliovirus for >20 years.
What is the nature of cell insult by polio virus?
Cytopathic effect - destroying cells
Which is the most affected parts of CNS?
Poliovirus can infect and destroy multiple sites of CNS
The primary site of insult are the anterior horn cells of SC and the cranial nerve nuclei in the medulla oblongata.
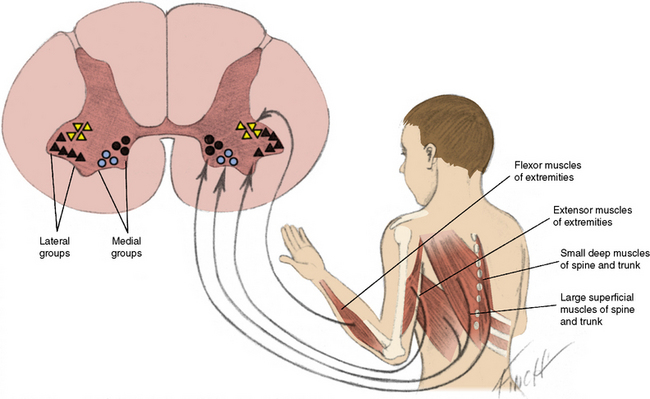
What happens d/t destruction of anterior horn cells in the spinal cord?
Lower motor neuron type of paralysis occur.
Because of the overlap in muscle innervation by 2-3 adjacent segments of the spinal cord, clinical signs of weakness in the limbs develop when more than 50% of motor neurons are destroyed.
What happens when medulla is involved?
Involvement if mild cause paralysis but if reticular formation catastrophic features d/t involvement of respiratory and autonomic centers.
What other parts of CNS can be affected in Polio?
Thalamus
Hypothalamus
DRG — causing myalgia, hyperaesthesia
What are findings in nerves of polio cases?
Perivascular inflammation involving PMNS, lymphocytes.
What are the findings in extra-CNS sites?
Hyperplastic lymphocytic follicles in tonsils & Peyer's patches
Inflammation in RES.
How can the vaccine polio be virulent?
Vaccine strains of polioviruses do not replicate in the CNS, a feature that accounts for the safety of the live-attenuated vaccine. Occasional revertants (by nucleotide substitution) of these vaccine strains develop a neurovirulent phenotype and cause vaccine-associated paralytic poliomyelitis (VAPP). Reversion occurs in the small intestine and probably accesses the CNS via the peripheral nerves.
Can we culture Poliovirus from the CSF of paralytic cases?
Not cultured till date.
Can patients with aseptic meningitis caused by poliovirus have paralytic disease?
Never
What helps in protecting human from polio?
Humoral and secretory immunity in the gastrointestinal tract is important for the control of enterovirus infections.
Capsid protein VP1 is the predominant target of neutralizing antibody, which generally confers lifelong protection against subsequent disease caused by the same serotype but does not prevent infection or virus shedding
Cellular immunity is also activated but significance is unknown.
Defect in humoral deficiency are likely to be at high risk than those with the abnormality in cellular immunity.
Is maternally derived immunity protective?
Maternally derived IgG and IgA provide protection for 4-6 months of life.
What are the ranges of clinical features of poliomyelitis?
Poliovirus infections with wild-type virus may follow 1 of several courses: inapparent infection, which occurs in 90–95% of cases and causes no disease and no sequelae;
abortive poliomyelitis;
nonparalytic poliomyelitis; or
paralytic poliomyelitis.
Paralysis, if it occurs, appears 3-8 days after the initial symptoms.
The ratio of asymptomatic to paralytic cases ranges from 50:1 to 1000:1.
What is abortive poliomyelitis?
Occurs in 5% cases
After 1-2 weeks of infection
Illness last for 2-3 days
Characterized by flu like symptoms - fever, myalgia, sore throat , abdominal pain, occasional vomiting.
Normal physical findings or may have pharyngitis and vague abdominal tenderness
Complete recovery without sequela
What is non-paralytic poliomyelitis?
Occurs in 1% of cases
Abortive polio symptoms with headache, nausea, vomiting.
Nuchal rigidity present
Basically features of aseptic meningitis
What is paralytic poliomyelitis?
Occurs in 0.1% cases
3 clinically recognizable syndromes that represent a continuum of infection differentiated only by the portions of the CNS most severely affected.
These are
(1) spinal paralytic poliomyelitis,
(2) bulbar poliomyelitis, and
(3) polioencephalitis.
How does spinal poliomyelitis manifest?
As a second phase of biphasic illness the first phase being symptoms of abortive phase.
Abortive phase like illness is followed by 2-5 days of apparent well being followed by second phase of deterioration.
How does the patient present with spinal poliomyelitis?
Spotty muscular involvement
Asymmetrical flaccid paralysis with single leg involvement being mc form followed by single arm involvement.
The proximal areas of the extremities tend to be involved to a greater extent than the distal areas.
Reduced muscle tone, fasciculations, muscle pain are often present.
Onset of paralysis occurs in febrile phase
Abdominal muscles, neck muscles, diaphragmatic , trunk and thoracic muscle are often involved.
Fleeting paralysis of bladder causing urinary retention and constipation are often present.
How long does it take for complete paralysis in paralytic cases?
24-48 hrs
What about reflexes in spinal polio?
Nuchal rigidity and exaggerated reflexes can preced the complete loss of superficial and deep reflexes.
Superficial reflexes are lost before deep reflexes.
What about sensory nervous system involvement?
Although patients complain of sensory symptoms objective sensory testing usually yields normal results.
What is the effect of IM injection and tonsillectomy on poliomyelitis?
Increases the risk of progression to paralysis
What happens to paralysis in defervescence?
The progression of paralysis stops after the fever subsides.
Little recovery from paralysis is noted in the 1st days or wk, but, if it is to occur, it is usually evident within 6 mo.
The return of strength and reflexes is slow and may continue to improve for as long as 18 mo after the acute disease.
Lack of improvement from paralysis within the 1st several wk or mo after onset is usually evidence of permanent paralysis. Atrophy of the limb, failure of growth, and deformity are common and are especially evident in the growing child.
What is bulbar poliomyelitis?
Although the 3 syndrome of polio is a continuum the term bulbar polio is reserved for cases that primary have bulbar symptoms.
What are the features of bulbar poliomyelitis?
Respiratory weakness along with weakness of extraocular, facial and masticatory muscles.
They also have
Nasal twang of voice
Nasal regurgitation of fluid and food
Dysphagia
Pooling of secretions in pharynx
Dysphonia, Aphonia, Hoarseness of voice d/t involvement of vocal cord
Deviation of palate, uvula and tongue.
Lack of effective cough
If respiratory centers and ANS are involved in medulla, can cause respiratory failure along with hypotension, Hypertension, arrhythmias .
Sometimes bulbar poliomyelitis can culminate into LAndry type ascending paralysis.
What is the rope sign?
The rope sign, an acute angulation between the chin and larynx caused by weakness of the hyoid muscles (the hyoid bone is pulled posteriorly, narrowing the hypopharyngeal inlet).
What is prognosis of bulbar poliomyelitis?
The course of bulbar disease is variable; some patients die as a result of extensive, severe involvement of the various centers in the medulla; others recover partially but require ongoing respiratory support, and others recover completely. Cranial nerve involvement is seldom permanent.
What is polioencephalitis ?
Rare
Encephalitis like features with extensive higher center of brain involvement.
Spastic paralysis with exaggerated reflexes with seizures, coma can be present.
Also they have flaccid paralysis
What is bulbospinal poliomyelitis?
When both bulbar and spinal involvement is present
What is paralytic poliomyelitis with ventilatory insufficiency?
Pure spinal poliomyelitis with respiratory insufficiency involves tightness, weakness, or paralysis of the respiratory muscles (chiefly the diaphragm and intercostals) without discernible clinical involvement of the cranial nerves or vital centers that control respiration, circulation, and body temperature. The cervical and thoracic spinal cord segments are chiefly affected.
Pure bulbar poliomyelitis involves paralysis of the motor cranial nerve nuclei with or without involvement of the vital centers.
Bulbospinal poliomyelitis with respiratory insufficiency affects the respiratory muscles and results in coexisting bulbar paralysis.
What are the impending signs of respiratory failure?
When the arms are weak, and especially when deltoid paralysis occurs, there may be impending respiratory paralysis because the phrenic nerve nuclei are in adjacent areas of the spinal cord. Observation of the patient's capacity for thoracic breathing while the abdominal muscles are splinted manually indicates minor degrees of paresis. Light manual splinting of the thoracic cage helps to assess the effectiveness of diaphragmatic movement.
How can we diagnose poliomyelitis?
The World Health Organization (WHO) recommends that the laboratory diagnosis of poliomyelitis be confirmed by isolation and identification of poliovirus in the stool, with specific identification of wild-type and vaccine-type strains.
In suspected cases of acute flaccid paralysis, 2 stool specimens should be collected 24-48 hr apart as soon as possible after the diagnosis of poliomyelitis is suspected.
Poliovirus concentrations are high in the stool in the 1st wk after the onset of paralysis, which is the optimal time for collection of stool specimens.
Polioviruses may be isolated from 80–90% of specimens from acutely ill patients in the first 2 weeks & in 20% cases in the 3rd week.
Because most children with spinal or bulbospinal poliomyelitis have constipation, rectal straws may be used to obtain specimens; ideally a minimum of 8-10 g of stool should be collected.
PCR of stool, CSF and body fluids have been used for diagnosis.
Serological methods have also been used for diagnosis
CSF finding in case of poliomyelitis?
The CSF is often normal during the minor illness and typically contains a pleocytosis with 20-300 cells/µL with CNS involvement. The cells in the CSF may be polymorphonuclear early during the course of the disease but shift to mononuclear cells soon afterward.
By the 2nd wk of major illness, the CSF cell count falls to near-normal values. In contrast, the CSF protein content is normal or only slightly elevated at the outset of CNS disease but usually rises to 50-100 mg/dL by the 2nd wk of illness.
What is the treatment of poliomyelitis?
No specific treatment
All IM injections and surgical procedures are contraindicated in the 1st week of illness as it may cause progression of illness
Abortive poliomyelitis - PCM, NSAIDS
Hot packs
For non-paralytic poliomyelitis -
Supportive
Hot packs
Splints
Avoid strenuous exercise
Flat beds
Management of paralytic poliomyelitis
Most patients with the paralytic form of poliomyelitis require hospitalization complete physical rest in a calm atmosphere for the 1st 2-3 wk.
Suitable body alignment is necessary for comfort and to avoid excessive skeletal deformity.
A neutral position with the feet at right angles to the legs, the knees slightly flexed, and the hips and spine straight is achieved by use of boards,sandbags, and, occasionally, light splint shells.
The position should be changed every 3-6 hr.
Active and passive movements are indicated as soon as the pain has disappeared.
Moist hot packs may relieve muscle pain and spasm.
Opiates and sedatives are permissible only if no impairment of ventilation is present or impending.
Constipation is common, and fecal impaction should be prevented.
When bladder paralysis occurs, a parasympathetic stimulant such as Bethanechol may induce voiding in 15-30 min; some patients show no response to this agent,and others respond with nausea, vomiting, and palpitations.
Bladder paresis rarely lasts more than a few days. If bethanechol fails, manual compression of the bladder and the psychologic effect of running water should be tried. If catheterization must be performed, care must be taken to prevent urinary tract infections.
An appealing diet and a relatively high fluid intake should be started at once unless the patient is vomiting. Additional salt should be provided if the environmental temperature is high or if the application of hot packs induces
sweating.
Anorexia is common initially.
Adequate dietary and fluid intake can be maintained by placement of a central venous catheter.
An orthopedist and a physiatrist should see patients as early in the course of the illness as possible and should assume responsibility for their care before fixed deformities develop.
The management of pure bulbar poliomyelitis consists of maintaining the airway and avoiding all risk of inhalation of saliva, food, and vomitus.
Gravity drainage of accumulated secretions is favored by using the head-low (foot of bed elevated 20-25 degrees) prone position with the face to 1 side.
Patients with weakness of the muscles of respiration or swallowing should be nursed in a lateral or semiprone position. Aspirators with rigid or semirigid tips are preferred for direct oral and pharyngeal aspiration, and soft, flexible catheters may be used for nasopharyngeal aspiration.
Fluid and electrolyte equilibrium is best maintained by intravenous infusion because tube or oral feeding in the 1st few days may incite vomiting.
In addition to close observation for respiratory insufficiency, the blood pressure should be measured at least twice daily because hypertension is not uncommon and occasionally leads to hypertensive encephalopathy.
Patients with pure bulbar poliomyelitis may require tracheostomy because of vocal cord paralysis or constriction of the hypopharynx; most patients who recover have little residual impairment.
What are the complications of paralytic poliomyelitis?
Complications d/t hypertension
Complications d/t immobilisation like Hypercalcemia, Nephrocalcinosis, ulcers
Deformity
Contractures
What is the prognosis of poliomyelitis?
Abortive and non-paralytic have good outcomes
Paralytic disease is determined primarily by degree and severity of CNS involvement.
In severe bulbar poliomyelitis, the mortality rate may be as high as 60%, whereas in less-severe bulbar involvement and/or spinal poliomyelitis, the mortality rate varies from 5% to 10%, death generally occurring from causes other than the poliovirus infection.
What are the risk factors a/w maximum paralysis?
Young male and adult female
IM injection
Tonsillectomy
Strenuous exercise in the early disease period
What is postpolio syndrome?
After an interval of 30-40 yr, as many as 30–40% of persons who survived paralytic poliomyelitis in childhood may experience muscle pain and exacerbation of existing weakness or development of new weakness or paralysis.
This entity, referred to as postpolio syndrome
What are the risk factors of Post polio syndrome?
Increasing length of time since acute poliovirus
Infection, presence of permanent residual impairment after recovery from acute illness, and
Female sex.
Click on the picture for VAPP and VDPV


Comments
Post a Comment